With PRP treatment against diabetes
Diabetic foot ulcers are the most common cause of leg amputations worldwide and there are several studies demonstrating the central role of altered granulation tissue formation in these chronic ulcers. It therefore seems reasonable that platelet-rich plasma (PRP) with multiple cytokines/growth factors may alter these sessile ulcers more rapidly during healing by closing the wound sooner and reducing the need for permanent amputations.
What foot problems are associated with diabetes?
If you have diabetes, it is important to check your feet regularly. You should see a podiatrist if any of the following problems occur:
- Blisters, wounds and cuts
- Corns and calluses.
- Nail fungus
- bunions and hammertoes.
- Plantar warts
- Athlete's foot
- Ingrown toenails
All these problems can get worse if they are not treated. If you cannot easily check your own feet, a doctor should help you.
How are diabetic foot ulcers treated?
Conventional treatments for diabetic foot ulcers include rest, bandaging, and topical and oral medications. A doctor can also determine if you are a candidate for platelet-rich plasma (PRP) injections, which have a high success rate in healing diabetic ulcers.
For these injections, he takes a blood sample, filters it and turns it to concentrate the platelets. The platelets contain essential growth factors for healing. The doctor then injects the PRP into areas of your body that need help to heal.
Does PRP help in the treatment of diabetic foot ulcers?
Diabetics have been found to have reduced tissue growth factor concentrations, especially epidermal growth factor. This deficiency impairs wound healing, leading to their chronic development and the risk of amputation. Diabetic ischaemic foot ulcers are the most difficult to treat and are associated with the highest risk of amputation.
Diabetics in combination with foot disorders often have a difficult clinical management. Such patients are prone to bone disease or a period of osteoarticular fusion surgery, mild to concomitant infections and difficult-to-heal skin ulcers.
Basic research has shown that the concentration of several important growth factors is significantly reduced at the site of diabetic foot injury. In recent years, it has been shown that in patients with diabetes who did not undergo Charcot art reconstruction, PDGF and VEGF levels at the bone fusion site were significantly lower than in normal individuals.
PRP contains several growth factors that are clinically related to the use of PRP therapy in Charcot joint reconstruction.
In a multicentre, prospective, clinical randomised controlled trial, Driver VR used autologous PRP gel to treat diabetic foot ulcers. A total of 40 eligible patients participated in the study. They were randomly divided into two groups: One treatment group received topical treatment with PRP gel. The control group received a saline gel treatment. Ulcer healing was assessed every 12 weeks for a total of 12 weeks. Thirteen (68.4%) and 9 (42.9%) ulcers recovered in the treatment and control groups, respectively. Kaplan-Meier time-to-cure analysis also showed that the PRP treatment group was significantly better than the control group. No serious side effects occurred during PRP treatment. The study concluded that the use of PRP was very effective for diabetic foot ulcers.
How does PRP therapy work?
PRP therapy can repair injuries and relieve pain in the body. It is associated with faster healing, a significant reduction in pain and a much lower risk than other treatments.
Growth factors and proteins are found in the platelets of the blood. These elements are designed to stimulate healing, support cell growth and generate new tissue. The body's first response to a soft tissue injury is to bring a rush of platelets to the site to speed up the repair process.
PRP therapy is a form of regenerative medicine that uses the natural healing powers of blood. The procedure involves extracting and isolating platelets and plasma from a sample of your own blood, then the doctor concentrates it in a healing solution. It is then injected back into the body at (and around) the point of injury or pain.
When the growth factors interact with local cells, they trigger the cells to heal the injury. This promotes tissue formation and reduces inflammation. The PRP solution can also provide a lubricating factor.
Summary
Diabetic foot ulceration is a major health problem and leads to amputation in 15%. There is a prolonged inflammatory phase that leads to a delay in granulation tissue formation and a decrease in the tensile strength of the wound. PRP improves wound healing by providing the necessary growth factors and reducing inflammation. Autologous PRP is a safe and cost-effective method of treating diabetic foot ulcers.
Related links
Treatment of a Non-Healing Diabetic Foot Ulcer With Platelet-Rich Plasma
Topical application of platelet-rich plasma for diabetic foot ulcers: A systematic review
Platelet-rich plasma for the treatment of diabetic foot ulcers: A meta-analysis
Platelet-rich plasma for the treatment of diabetic foot ulcer: a randomized, double-blind study
Related topics

PRP and temporomandibular joint disorders (TMD): A new treatment perspective?
The use of PRP for temporomandibular joint disorders could represent a new treatment option. How does this therapy work and what do the latest studies say?
Read more
PRP and neuroregeneration: potential for strokes and neurological diseases
The use of PRP in neurological diseases such as strokes is an exciting field of research. What progress has been made in neuroregeneration?
Read more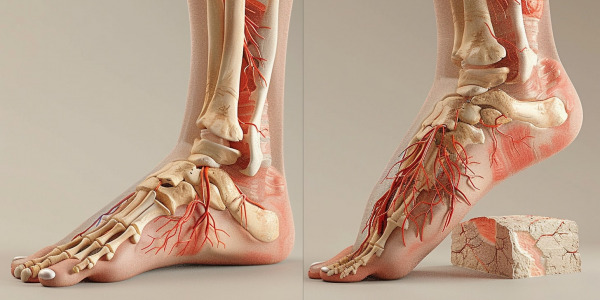
PRP in podiatry: treatment of heel spurs and foot pain
More and more podiatrists are using PRP to treat heel spurs and chronic foot pain. What are the latest findings in this area?
Read more
Dyspareunia-PRP quality of life: a comprehensive overview
Discover how PRP therapy relieves dyspareunia and improves quality of life. Learn more about symptoms, treatments and patient experiences.
Read more
Endometrial problems and the revolutionary role of PRP treatment.
Endometrial problems can be a challenge for women trying to conceive, with thin endometrium posing a particular difficulty. PRP treatment, a method that uses platelet-rich plasma from the patient's own blood, shows promising results in treating endometrial problems.
Read more
Ovarian Insufficiency and PRP Therapy
PRP therapy is a relatively new treatment option for ovarian insufficiency. In this therapy, the body is injected with an autologous plasma preparation enriched with a high concentration of growth factors. These growth factors can stimulate the ovaries and improve egg production.
Read more
Restoration of tubal function with platelet rich plasma
In recent years, the use of PRP to improve ovarian function in women with premature ovarian failure or low ovarian reserve has also been explored. The results of some studies suggest that PRP can increase the number and quality of eggs and improve pregnancy rates.
Read more
Dermaroller and its application: synergies with PRP, serums and hyaluronic acid.
Dermaroller is specifically designed to stimulate the natural regeneration of the skin and is increasingly used in combination with other treatments such as PRP, serums and hyaluronic acid.
Read more
FAQ - PRP training in the areas of trichology, orthopedics and aesthetics.
PRP training in the areas of trichology, orthopedics, and aesthetics is a hands-on, limited time, small group training that specializes in the application of PRP in these areas.
Read more
Your blood. Your power. PRP Penile Injection.
In our latest blog article, we highlight the innovative possibilities of PRP penile injections. What's behind the platelet-rich plasma trend, and how can it help men improve their sexual function? In addition to a detailed look at the procedure and potential benefits of the treatment, we also address potential risks and side effects.
Read more
Applications of PRP in animals: An overview
In this article, we will provide an overview of the applications of PRP in animals and how it can help improve their health.
Read more
Why are platelets of interest to dermatologists?
Platelets are small, seedless blood platelets that play an important role in blood clotting. They can be involved in various skin diseases such as wounds, inflammation or bleeding.
Read more
Required equipment and consumables for PRP treatment
A PRP treatment requires special equipment and consumables. These include a centrifuge, tubes, syringes and needles.
Read more
Lipolysis treatment: A modern way to the dream figure.
Welcome to our comprehensive guide to lipolysis treatment. Are you looking for an effective, minimally invasive method of fat reduction? Then you might be in the right place.
Read more
PRP training: practice upgrade?
The increasing popularity of natural methods of aesthetic medicine has led to the increased use of platelet-rich plasma (PRP). Aesthetic medicine specialists can broaden their horizons and enhance their practice with PRP training. This blog post addresses the benefits of such PRP training.
Read more
PRP aesthetics for men
PRP (platelet-rich plasma) aesthetics is an up-and-coming aesthetic treatment that is becoming increasingly popular, especially among men. In this article, we take a closer look at this innovative method and why it's ideal for men.
Read more
PRP treatments in veterinary medicine: a promising prospect for the future
Platelet rich plasma (PRP) treatments are a promising future prospect in veterinary medicine. Platelet therapy has been established in both veterinary and human medicine for the treatment of poorly perfused tissues.
Read more
Autologous blood therapy for hair
Autologous blood therapy is an innovative and safe treatment method that is becoming increasingly popular for hair loss and thinning hair.
Read more
Can PRP be combined with biorevitalization?
Are PRP and biorevitalization compatible with each other? The preparations act on different processes in the body and complement each other perfectly.
Read more
PRP injections for lips
A PRP treatment for lips consists of a painless injection of platelet-enriched plasma into the skin. The resource for the procedure is the patient's blood, from which platelets are obtained in a concentrated form. These are responsible for stimulating cellular functions and inhibiting the aging process.
Read more
Questions and answers about carboxytherapy
The main cause of aging of the epidermis is a lack of oxygen in the tissues.
Read more
Answers to frequently asked questions about PRP treatment
What is PRP treatment? It is a medical technology that uses an injectable form of autoplasm derived from blood platelets.
Read more
PRP therapy: its therapeutic properties
PRP therapy is an injectable procedure in which a patient's platelet-rich plasma is injected into a body part that requires rapid healing, i.e., it is intended to accelerate regeneration and stimulate the growth of the body's own cells.
Read more
Saving Lives: Blood Plasma
Blood plasma is a versatile drug with pronounced detoxifying and hemostatic properties. It has various functions (nutrition, transport, buffering and others).
Read more
PRP nebulizer for lung diseases - an innovative treatment method
One of the most serious effects of coronavirus disease (COVID19) is lung diseases such as acute respiratory distress syndrome. In the absence of effective treatments, it is necessary to search for new therapies and therapeutic targets. Platelets play a fundamental role in respiratory diseases derived from viral infections, as they are the first line of defense against viruses and are essential for maintaining lung function.
Read more
What is regenerative medicine?
Regenerative medicine encompasses many different innovative therapies whose goal is autologous (the body's own) tissue regeneration.
Read more
PRP treatment in sports medicine
PRP is an agent used to biologically stimulate tissue healing. It can be an effective method of treating sports injuries and is therefore becoming increasingly popular. PRP procedure can and should play an important role in solving the most current orthopedic problems in the present and in the future!
Read more
PRP treatment for rosacea
PPR allows the skin to rejuvenate and repair itself, which can help relieve and calm the symptoms of rosacea.
Read moreTreatment of cellulite with PRP (platelet rich plasma)
In the modern world, 90% of women struggle with body blemishes (cellulite, stretch marks). The introduction of autologous platelet plasma can reduce the severity of these defects and improve the quality and appearance of the skin.
Read moreHair Loss Support and Treatment
Hair loss, also called alopecia, is complete or partial baldness due to hormonal changes or physical or psychological stress.
Read more
FUE hair transplantation
FUE transplants are the most common and successful method of curing hair loss. Find out more about the FUE hair transplant process.
Read more
You want to make plasma gel? What equipment do you need to do this?
We are often asked what equipment is needed for plasma gel? You will find an answer in this article.
Read morePlasma growth factors in cerebral palsy
The use of plasma growth factors has opened up a new clinical field of application in medicine and given rise to a new discipline called regenerative medicine. In many areas such as traumatology, dental implants or anaesthesia, the use of this biotechnology can improve patients' quality of life.
Read more
PRP therapy for tendonitis
Repetitive movements can stretch tendons and cause pain, swelling and limited movement. Try PRP therapy to perform tendon repair, which can heal hard tissue and not just mask pain and cause long-term damage like traditional treatments.
Read moreLearn more about PRP treatment: how it works and what it does.
PRP treatments are an innovative technique that helps improve skin quality and treat certain skin conditions. These treatments are safe, gentle and effective and can help improve the appearance and condition of the skin. Learn more about PRP treatments, how they work, and what results you can expect.
Read moreCan carpal tunnel syndrome be treated with PRP therapy?
Carpal tunnel syndrome (CTS) is a condition that affects a patient's quality of life. About three to six percent of the adult population in the United States suffers from carpal tunnel. Some cases of CTS improve on their own, but many require medical intervention. Unfortunately, many modern medical treatments offer only short-term relief for patients. They do not solve the underlying problem that causes CTS.
Read morePRP or dermal filler - Which should I choose?
People of all ages are concerned with combating various signs of skin ageing. Some of the most popular options for patients are injectables such as dermal fillers and platelet-rich plasma injections. These two are non-surgical enhancement techniques that help you look younger than your actual age.
Read morePRP treatment after hair transplantation
PRP treatment after hair transplantation is used to promote faster wound healing and hair growth after hair transplantation. PRP treatment is said to help revitalise weak hair follicles that are prone to falling out. It has been observed that the hair in the treated area is less thin and the hair shafts are thicker in patients treated with PRP.
Read moreWhat is the effect of PRP therapy in orthopaedics?
In recent years, various methods of using platelet-rich plasma (PRP) have been applied during the treatment of various orthopaedic diseases and sports traumas. They enable the improvement of the local biological condition and the regeneration of different tissue types. PRP is a modern treatment strategy with worldwide recognition.
Read morePlatelet-rich plasma: the key to PRP therapy
Platelet-rich plasma (PRP) is used in a variety of clinical applications based on the premise that higher GF content should promote better healing. Platelet derivatives represent a promising therapeutic modality and offer possibilities for the treatment of wounds, ulcers, soft tissue injuries and various other cell therapy applications.
Read moreDoes PRP treatment work for hair loss?
Platelet-rich plasma (PRP) is a treatment that doctors use to speed up healing in different areas of the body. It can help restore hair growth. Doctors usually use this treatment for hair loss results from androgenetic alopecia, a common condition that causes hair follicles to shrink.
Read morePRP treatment against melasma
There is no shortage of treatments to "cure" melasma, but unfortunately many of them do not work and simply rob clients of time, money and emotional stress. Platelet-rich plasma (PRP), however, offers promising treatment options for people living with melasma. Let's first discuss the disease and how PRP can help with the condition.
Read more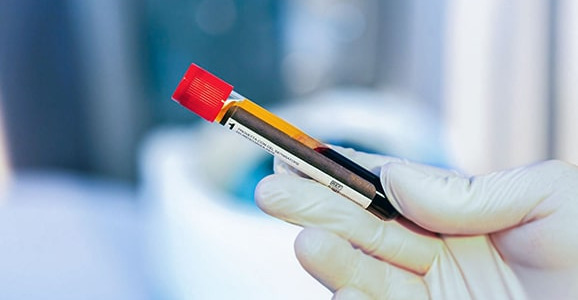
What are PRP tubes?
Platelet-rich plasma, better known as PRP, is an autologous procedure in which a person's whole blood is drawn. The platelets are then concentrated using a centrifuge and special PRP tubes. The platelets, which contain several growth factors, are then taken again -in this feature injected into the same person makes PRP alone a very safe procedure that eliminates the likelihood of contracting communicable diseases.
Read morePhotodynamic therapy (PDT)
Photodynamic therapy (PDT) is a treatment that involves light-sensitive drugs and a light source to destroy abnormal cells. It can be used to treat some skin and eye diseases as well as certain types of cancer .
Read moreLipogems / Lipogems Treatment
Lipogems is a medical device that extracts fat (also called adipose tissue) from your abdomen and injects it into your arthritic and/or painful joint. This helps relieve joint pain and allows you to regain function and return to your daily activities.
Read morePRP treatment of diabetic foot ulcers and wounds
PRP treatment of diabetic foot ulcer is effective and safe. PRP is effective if it significantly accelerates the healing of the diabetic foot ulcer and safe if it does not cause significant changes in the patient's blood haematology or blood chemistry (albumin).
Read morePRP therapy for back pain
By injecting PRP directly into the lower back, these growth factors and proteins are concentrated exactly where they are needed so they can begin to heal and repair damaged areas to relieve pain and restore normal spinal function.
Read morePlatelet Rich Plasma (PRP) for brain injuries
PRP is rich in numerous growth factors associated with the repair processes following injury to the central nervous system, which consists of the brain and spinal cord.
Read moreThe most common sports injuries that can be treated with PRP.
Many sports injuries improve with platelet-rich plasma (PRP) injections. Both professional athletes and weekend warriors can be out due to injuries. Athletes have traditionally had the choice of either sitting out for weeks or months to heal or undergoing major surgery - neither of which is particularly desirable. PRP injections offer a radical third alternative. This minimally invasive, safe and fast orthobiological treatment is highly effective for many of the most common sports injuries.
Read morePRP in gynaecology - Vaginal rejuvenation
PRP can be extremely beneficial for vaginal rejuvenation. As platelets are responsible for both promoting healing and regenerating healthy tissues in your body, PRP can be an ideal solution if you are looking for a vaginal treatment with rejuvenating properties. Depending on your needs, PRP injections can be performed into the tissues surrounding the clitoris, urethra and G-spot. When injected into the areas targeted for treatment,
Read morePRP treatment for wrist pain
Hands and wrists are amazingly complex, with 27 bones, a complex network of ligaments, tendons, joints, nerves and muscles working gracefully together. The human hand can type across a keyboard, serve a tennis ball, turn a doorknob and feel the gentle touch of a child's hand. If you are suffering from an injury to the ligaments or tendons in your hands, wrists or elbows, a PRP injection can speed up the healing process. Your doctor may use a PRP injection with surgery to help you recover faster.
Read more
Why should you offer PRP injections in your medical practice?
PRP is used in almost every field and specialty, from sports medicine to pain management, skin rejuvenation, hair care and urology. Most doctors who use this treatment also saw higher patient retention rates. So is there a legitimate reason not to add PRP to your practice?
Read morePRP (Platelet Rich Plasma) in cardiac surgery
PRP is a safe, simple and reproducible therapy that appears to offer both clinical and financial benefit to patients undergoing sternotomy for cardiac surgery. The addition of PRP to all sternal occlusions following cardiac surgery brings value by improving care and reducing costs.
Read morePRP (Platelet Rich Plasma) treatment for COPD disorders
PRP treatments for COPD conditions can help repair the air sacs or alveoli and reverse lung damage caused by smoking, pollution and other factors. Make breathing easier, relieve chest discomfort and increase stamina with PRP therapy.
Read more
PRP treatment for periodontal disease
Inflammatory periodontal disease is one of the most pressing problems in dentistry, which is not only of general medical but also of social importance.
Read morePRP (Platelet Rich Plasma) therapy in dermatology
Platelet-rich plasma (PRP) is an autologous serum containing high concentrations of platelets and growth factors. PRP therapy continues to evolve as an important treatment modality with many applications in dermatology, particularly in the areas of hair restoration, skin rejuvenation, acne scars, skin augmentation and striae distensae. In addition, the combination of PRP with laser therapies, microneedling, dermal fillers and autologous fat grafting leads to synergistic effects that result in improved aesthetic outcomes.
Read moreUse of PRP (Platelet Rich Plasma) therapy in dogs with pain.
Is your dog recovering from an injury or suffering from degenerative joint disease? Platelet-rich plasma therapy (PRP) can help.
Read more
PRP (Platelet Rich Plasma) treatment for coccygodynia
Try PRP for coccydynia or tailbone pain, a condition for which there are no conventional remedies apart from treatments to relieve symptoms. Gain a better quality of life with the ability to sit pain-free and need support.
Read more
PRP treatment for shoulder pain
In the orthopaedic community, the clinical use of PRP (platelet-rich plasma) in the treatment of shoulder pathologies has increased rapidly over the last decade.
Read more
Microneedling for acne scars
As if acne is not frustrating enough, sometimes you have to deal with the scars that acne may leave. Acne scars may appear due to cystic acne or itchy skin. Like other types of scars, acne scars can last for months or longer. Even a few years. Want to learn more about microneedles for acne scars? Read on to learn more about the procedure and discuss its effectiveness and possible side effects with your dermatologist.
Read morePRP (Platelet Rich Plasma) therapy for plantar fasciitis
Recently, platelet-rich plasma (PRP) has been used as an alternative therapy for plantar fasciitis (PF) to relieve heel pain and improve functional recovery.
Read more
What are platelet rich plasma (PRP) injections?
Times have changed since the days of bloodshed, when doctors treated their patients by drawing blood from them. Now a procedure called platelet-rich plasma therapy has emerged in which some of the blood is injected back into a diseased joint. You could say it's bloodshed in reverse.
Read more
Does PRP therapy help with tennis elbow?
Platelet-rich plasma (PRP) therapy uses the body's own natural healing processes to repair damaged tissue. Platelets are blood cells that promote blood clotting and support wound healing. PRP contains many proteins called growth factors (more than normal blood) that help the tendon to heal and consequently relieve your pain.
Read morePRP progress: Why you as a medical professional should offer this treatment.
Platelet-rich plasma (PRP) has received considerable attention in the field of dermatology since the elucidation of its mechanism and reports of its clinical efficacy. PRP alone or in combination with other therapies has shown benefits for some cosmetic problems and skin conditions. Few transient or short-term side effects have been reported with the use of PRP. In this paper we highlight the potential efficacy and benefits of PRP
Read morePRP therapy for eye diseases
Blood products (autologous serum, platelet-rich plasma (E-PRP), plasma rich in growth factors) are successful therapies for ocular surface diseases that affect the integrity of the corneal surface and conjunctiva.
Read more
PRP treatment for knee pain
Does PRP treatment work for knee pain? Platelet-rich plasma (PRP) injections are a novel treatment for pain associated with osteoarthritis of the knee.
Read more
PRP treatment for erectile dysfunction
Platelet-rich plasma (PRP) found its use in the treatment of various conditions and diseases, as concentrated plasma PRP consists of many growth factors. Their interaction with surrounding cells, intracellular matrix and mediators at the injection site leads to tissue regeneration. Angiogenic, vasculogenic and regenerative effects of PRP can be used to treat erectile dysfunction (ED) and Peyronie's disease (PD).
Read more
PRP injection or cortisone injection? - Which is the best option?
Before the development of PRP (platelet-rich plasma) injections, doctors generally used cortisone injections to relieve moderate to severe muscle / joint inflammation and (some) pain. However, with the creation of PRP injections, doctors can now relieve inflammation and pain as well as help the damaged tissue heal.
Read moreThe right care after PRP treatment
If you have PRP therapy applied as a topical serum for skin problems, your doctor will probably recommend no strenuous physical activity or exercise for about 48 to 72 hours after treatment. Recommendations may differ for other PRP applications, including orthopaedic injuries and hair loss. The best way to ensure proper healing and ideal results is to follow your provider's post-operative guidelines closely, including temporarily interrupting your exercise routine if recommended.
Read more
PRP Tubes | Vi PRP-PRO Set
PRP tubes | Vi PRP-PRO set with separating gel and anticoagulant. Platelet-rich plasma (PRP) therapy is an innovative treatment that stimulates the body's natural healing process and utilizes the patient's own cells to promote accelerated healing of certain musculoskeletal disorders, sports injuries and arthritic joints. It provides powerful growth factors that stimulate and enhance the blood supply to the injured area and the nutrients cells need to regenerate damaged tissue.
Read more
Treat dark circles with Vampire Lift / PRP therapy
Injecting the platelet-rich plasma under the eyes gives the skin below the eye the vital nourishment it needs. Once injected into your skin, the platelets promote the growth and regeneration of your own collagen, resulting in increased smoothness and firmness of the skin.
Read morePRP therapy for injury scars
PLATELET GROWTH FACTORS derived from blood (plasma) and responsible for repair processes can regenerate the skin in injury scars. The concentration of platelet growth factors in platelet-rich plasma (PRP) is about 95%, compared to only 4 to 5% found in normal-forming clots. Therefore, PRP can stimulate tissue regeneration much faster than normal.
Read moreWound healing through PRP therapy
Many elements such as cytokines and growth factors are involved in the regeneration process of injured tissues. The growth factors contained in platelets represent an important physiological mixture of factors that may be involved in the healing process.
Read morePRP treatment for acne
Platelet-rich plasma is injected into the acne-damaged area of the face to stimulate the production of new collagen and elastin, reduce the appearance of scars, and make the skin look brighter and smoother.
Read more
Density Platelet Gel - PRP-Tubes
Density Platelet Gel - PRP tubes for your PRP treatments.
Read more
PRP injection for facial beautification
Is platelet-rich plasma the secret to younger-looking skin? What exactly are PRP injections for facial beautification?
Read morePRP skin treatments
The body cells that help tissues heal and produce new cells are called platelets. PRP is injected into specific areas of the skin and then creates an environment that helps with the growth of collagen, regenerates tissue and makes your skin smooth and firm. PRP reduces wrinkles and creates a skin texture and tone that is smoother, younger and better.
Read morePRP treatment for hair loss - questions and answers
PRP therapy for hair loss is also known as platelet-rich plasma therapy . It is a treatment offered to men and women of all ethnicities. It is a simple, non-surgical procedure in which the patient's PRP is extracted by drawing blood and separating the platelet-rich plasma from the rest of the blood using a centrifuge. The plasma is then injected into the thinning areas of the scalp to stimulate hair growth and provide fuller, healthier looking hair.
Read more

